Clinical utility of a digital health agent to deliver motivational interviewing to treat alcohol abuse
Title: Clinical utility of a digital health agent to deliver motivational interviewing to treat alcohol abuse.
Authors: Jaynish Hazari, MPH, MA; Maya Boustani, PhD; Christine Lisetti, PhD
Keywords: Digital health, Utility, Virtual health agent
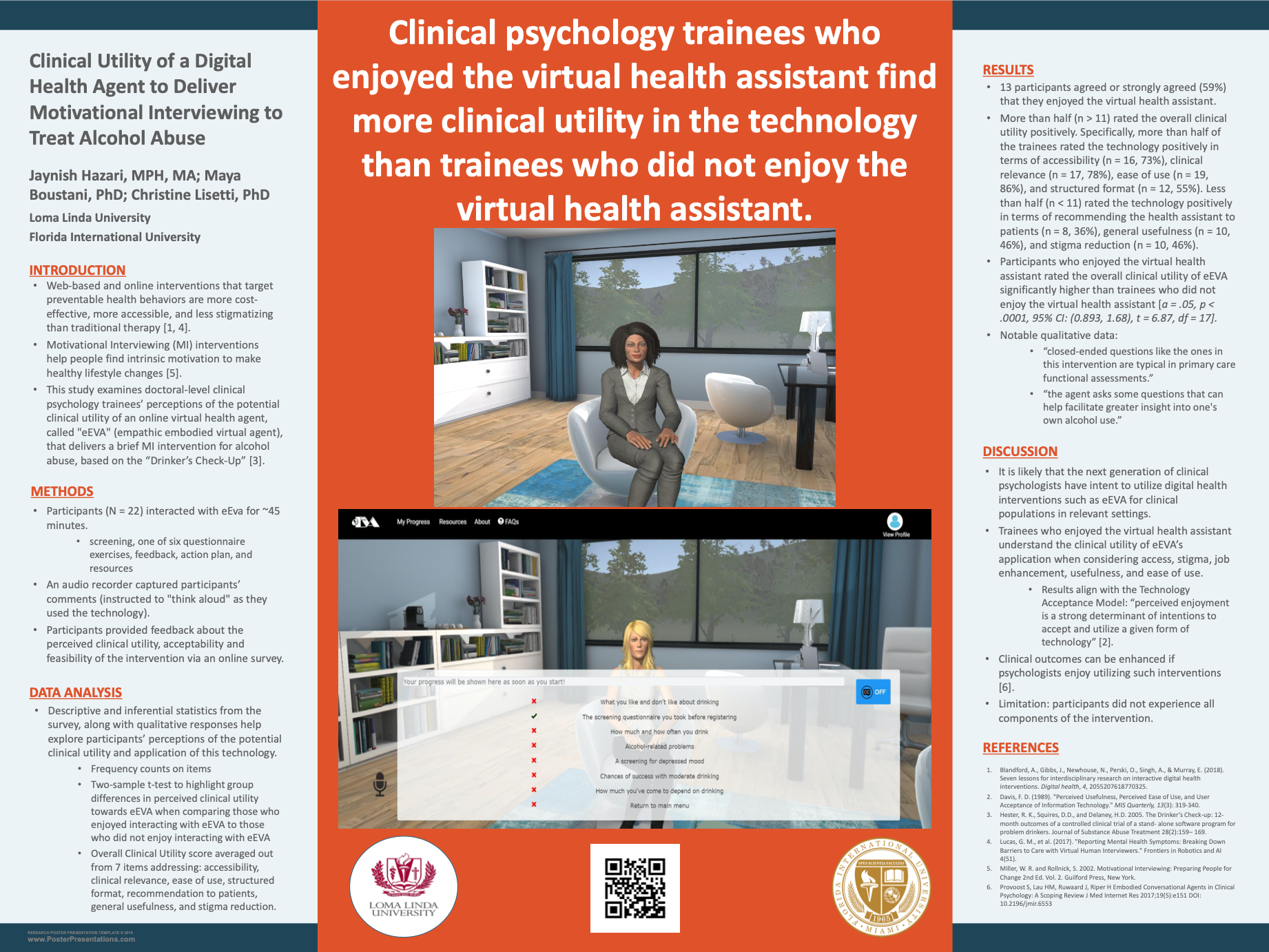
BACKGROUND: Web-based and online interventions that target preventable health behaviors and are based on evidence-based therapies such as Motivational Interviewing (MI) are more cost-effective, more accessible, and less stigmatizing than traditional therapy (Blandford et. al., 2018). This study examines doctoral-level clinical psychology trainees’ understanding and perception of the potential clinical utility of an online virtual health agent, called "eEVA" (empathic embodied virtual agent), that delivers a web- based MI intervention for alcohol abuse. MI-based interventions have shown to help people find intrinsic motivation to make healthy lifestyle changes (Miller & Rollnick, 2002). The current study examines clinical psychology trainees’ impressions and satisfaction of eEVA, focusing on the perceived clinical utility of this technology for patients who may be at risk for alcohol problems, as literature indicates that digital health user satisfaction is a strong predictor of patients meeting desired clinical goals and outcomes (Provoost et. al., 2018).
METHODS: After interacting with eEva for 30-45 minutes, 22 doctoral-level clinical psychology trainees with clinical experience provided feedback about the perceived clinical utility of the intervention via an online survey. An audio recorder captured participants comments, as they were instructed to "think aloud" as they used the technology. Participants completed a post-intervention questionnaire based on a combination of O’Brien’s 6-attribute model, Heerink’s model and Bartneck's ‘Godspeed questionnaire’ to determine the acceptability, feasibility, and usefulness of EEVA. Descriptive statistics and frequency counts from the survey, along with written qualitative responses help explore participants’ perceptions of the potential utility and application of this technology.
RESULTS: A majority of participants agreed or strongly agreed (78%) that the agent could be relevantly useful for patients with alcohol abuse issues, stating that the agent “asks some questions that can help facilitate greater insight into one's own alcohol use”. Also, most agreed or strongly agreed (73%) that they would recommend the agent to patients who do not have access to receive help from a live health assistant. Participants largely disagreed or strongly disagreed (73%) that the agent was a threat to their job security. Furthermore, most of them (86%) agreed that the agent was easy to use. Clinical psychology trainees had mixed feedback about the potential for eEva to reduce stigma associated with seeking help. About 46% agreed or strongly agreed that individuals would be more truthful stating that "this could be a possibility,” 27% neither agreed nor disagreed stating “ I don't think there would be a difference,” and 28% disagreed or strongly disagreed stating “ It depends on the person.” Other qualitative data revealed that "closed ended questions like the ones in this intervention are typical in primary care functional assessments," which could be a potential clinical application of its utility.
CONCLUSION: The innovations in empathic virtual health agents represent an enabling form of health technology for a variety of applications relevant to a wide range of public health issues. In the current study, the next generation of clinical psychologists appear to view the technology favorably regarding its clinical utility and applications, and do not seem threatened by it. Although this sample does not fully agree that it can help patients be more truthful about their alcohol use, the literature indicates otherwise, with studies showing that overcoming problems of stigma has been traditionally considered a major benefit of internet-delivered and computer-based health interventions (Lucas et. al., 2017). Furthermore, participants seemed favorable to the idea of using such technology to supplement their delivery of care in both community and healthcare settings. Future directions include examining the feasibility, acceptability, and effectiveness of using this technology with individuals experiencing alcohol abuse.
References:
Lucas, G. M., et al. (2017). "Reporting Mental Health Symptoms: Breaking Down Barriers to Care with Virtual Human Interviewers." Frontiers in Robotics and AI 4(51).
Miller, W. R. and Rollnick, S. 2002. Motivational Interviewing: Preparing People for Change 2nd Ed. Vol. 2. Guilford Press, New York.
Provoost S, Lau HM, Ruwaard J, Riper H Embodied Conversational Agents in Clinical Psychology: A Scoping Review J Med Internet Res 2017;19(5):e151 DOI: 10.2196/jmir.6553